Report: 100 Healthcare Execs Speak Out On Using AI To Curb Fraud, Waste And Abuse

 In June of this year, a jury found a chiropractor guilty of defrauding health insurers out of $2.2 million by fraudulently billing for services that were never provided, and even went out of her way to issue bogus medical diagnoses, write false prescriptions and bill for fake office visits that never happened.
In June of this year, a jury found a chiropractor guilty of defrauding health insurers out of $2.2 million by fraudulently billing for services that were never provided, and even went out of her way to issue bogus medical diagnoses, write false prescriptions and bill for fake office visits that never happened.
This is an example of cases that are causing a rise in concern for fraud, waste and abuse (FWA) schemes which are becoming rampant in the healthcare space and costing health insurers nearly 12 percent of their annual revenues, according to recent PYMNTS research. FWA is leading to significant problems that are plaguing claims management, payments and the overall cost of accessing healthcare.
Health insurers ha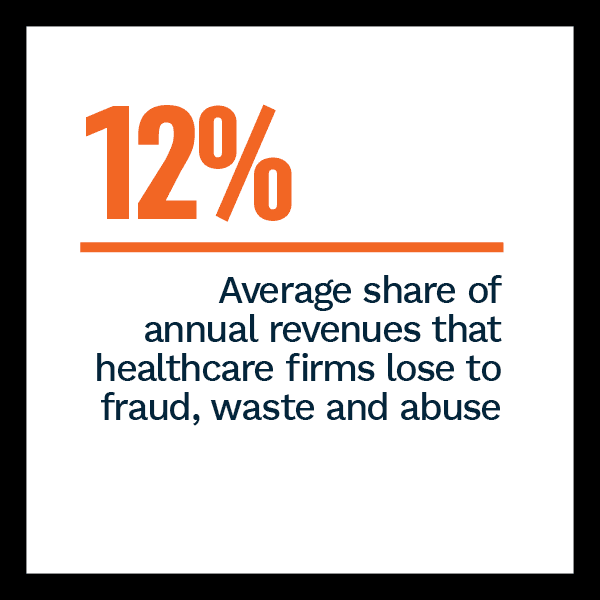 ve a responsibility to their stakeholders, including both corporate employers and their employees, to prevent sharp increases in rates and other out-of-pocket expenses. Claims departments at insurance companies can find themselves playing whack-a-mole as new FWA schemes regularly continue to pop up.
ve a responsibility to their stakeholders, including both corporate employers and their employees, to prevent sharp increases in rates and other out-of-pocket expenses. Claims departments at insurance companies can find themselves playing whack-a-mole as new FWA schemes regularly continue to pop up.
As insurers are cognizant of the problem and are actively turning to solutions that can help them tackle FWA, however, PYMNTS’ research reveals that 44 percent of larger firms surveyed have already invested in artificial intelligence (AI) to combat FWA, while 71 percent who are currently not using AI are looking to invest in AI in the next one to three years to improve payments integrity.
AI In Focus: Targeting Fraud, Waste And Abuse In Healthcare, a collaboration between PYMNTS and Brighterion, a Mastercard company, offers an overview of the challenges and responsibilities healthcare insurers have faced over the past year and why they are bri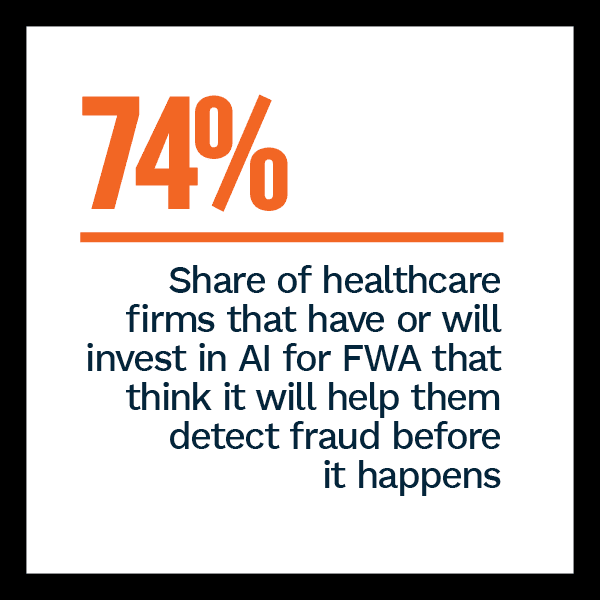 nging FWA to the forefront. Our analysis is based on a survey of 100 healthcare executives that either have intimate knowledge or hold leadership responsibilities in fraud detection and analysis, financial planning and analysis, claims payments or risk management.
nging FWA to the forefront. Our analysis is based on a survey of 100 healthcare executives that either have intimate knowledge or hold leadership responsibilities in fraud detection and analysis, financial planning and analysis, claims payments or risk management.
Some healthcare firms have applied payment integrity practices for accuracy checks and reducing the likelihood of errors, but this approach served as problematic, as 54 percent of healthcare insurance respondents apply payment integrity practices when analyzing payments from providers but do not do so for payments from consumers.
Surveyed firms also cite a variety of reasons for implementing AI, yet those of all shapes and sizes unanimously agree that reducing false positives is a key benefit. Eighty-three percent of surveyed firms that have or will invest in AI to detect FWA consider reducing false positives as the most important expected benefit and 66 percent of healthcare executives believe that an AI tool’s accuracy in reducing false positives is the most important factor when picking a provider.
However, there 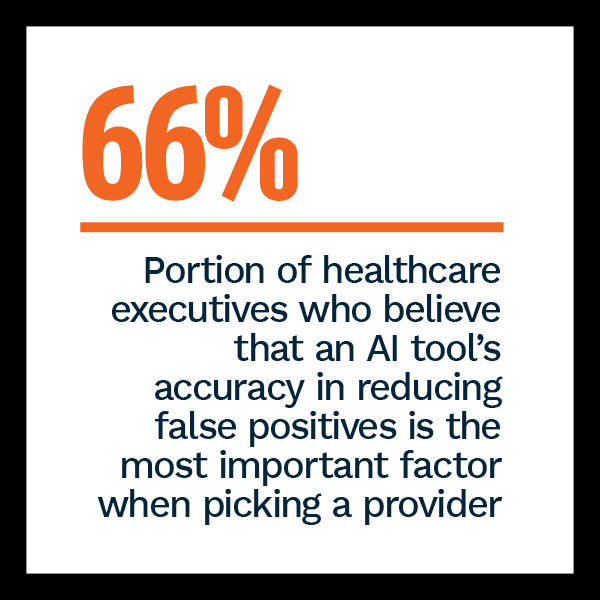 are still several barriers to the adoption of AI tools that can help healthcare insurers improve payment integrity. Chief among these barriers is the high data management cost that is associated with the implementation of AI tools, as 68 percent of surveyed firms cite it as the most important challenge. This is notably the case for the 83 percent of firms that generate less than $100 million in annual revenue. That share is almost twice as much for firms that generate more than $1 billion in annual revenue. Seventy-four percent of healthcare firms that have or will invest in AI to detect FWA expect AI will help them detect fraud before it happens.
are still several barriers to the adoption of AI tools that can help healthcare insurers improve payment integrity. Chief among these barriers is the high data management cost that is associated with the implementation of AI tools, as 68 percent of surveyed firms cite it as the most important challenge. This is notably the case for the 83 percent of firms that generate less than $100 million in annual revenue. That share is almost twice as much for firms that generate more than $1 billion in annual revenue. Seventy-four percent of healthcare firms that have or will invest in AI to detect FWA expect AI will help them detect fraud before it happens.
These findings touch upon just a few of the insights outlined in our research. To learn more about how healthcare firms plan to combat FWA, download the report.
